Plantar Fasciitis, Per Cavus, and You: Choosing the Right Footwear
- Aria

- May 3, 2025
- 4 min read
Updated: Jun 11, 2025
Foot pain is more than just a nuisance—it’s a disruption to your daily life, mobility, and overall well-being. While a sore foot after a long day may not seem like much, consistent discomfort could be pointing to underlying structural issues like Plantar Fasciitis or Per Cavus. These two conditions, though very different in nature, are united by one common need: the right footwear.
In this comprehensive guide, we’ll explore what these conditions are, why proper shoes matter, and how you can make smarter choices to protect your feet—step by step.
Understanding Your Feet: An Introduction
Your feet are complex mechanical structures, each comprising 26 bones, 30 joints, and more than 100 muscles, tendons, and ligaments. They absorb shock, support your body weight, and help maintain balance. Any misalignment or stress in this system can result in chronic pain or long-term damage.
Two of the most common structural foot concerns that demand attention are:
Plantar Fasciitis – often linked with heel pain and inflammation
Per Cavus – a condition marked by excessively high arches
Let’s look at both in depth.
What is Plantar Fasciitis?
Plantar Fasciitis is the inflammation of the plantar fascia—a thick, fibrous band of tissue running along the bottom of your foot from the heel to the toes. This condition is most often associated with stabbing pain in the heel, particularly during the first steps after waking up or prolonged inactivity.
Symptoms
Sharp pain in the heel or mid-foot
Morning foot stiffness
Pain worsening after exercise
Swelling or warmth in the arch area
Causes
Flat feet or overly high arches
Tight Achilles tendons
Poor footwear with minimal arch support
Prolonged standing or running on hard surfaces
Obesity or rapid weight gain

What is Per Cavus?
Per Cavus, also called high-arched foot, refers to a condition where the arch of the foot is significantly higher than normal. This alters the natural alignment of the foot, shifting the body’s weight to the ball and heel, rather than allowing for even distribution.
Symptoms
Pain while walking or standing
Ankle instability or frequent sprains
Calluses on the ball, heel, or outer edge of the foot
Clawed toes
Rigid foot structure
Causes
Can be hereditary
May develop from neurological disorders like Charcot-Marie-Tooth disease or polio
In some cases, the cause is idiopathic (unknown)

The Impact of Poor Footwear
Choosing the wrong footwear is often the silent culprit behind aggravated foot conditions. Whether it's lack of cushioning, poor arch support, or improper heel elevation, many modern shoes are more about fashion than function.
For both Plantar Fasciitis and Per Cavus, improper shoes can:
Increase heel pressure and pain
Exacerbate arch tension
Limit mobility and worsen gait alignment
Cause additional injuries like Achilles tendonitis or metatarsalgia
Footwear Features That Matter
If you’ve been diagnosed with either of these conditions—or suspect you might be dealing with them—the right footwear is not optional. It’s essential.
Here’s what to look for:
1. Adequate Arch Support
For Plantar Fasciitis, good arch support reduces the strain on the plantar fascia.
For Per Cavus, it helps distribute weight evenly to prevent pressure sores and balance issues.
2. Cushioned Insoles
Extra cushioning absorbs impact and provides comfort during long periods of standing or walking.
3. Heel Support
A slightly elevated, well-padded heel reduces the stretch on the plantar fascia.
A stable heel counter helps prevent ankle rolls in people with Per Cavus.
4. Wide Toe Box
Provides room for natural toe splay, especially important for high-arched feet or claw toes.
5. Shock Absorption
Essential for both conditions to reduce the impact on heel and metatarsal heads.
6. Firm Midsole
A stiff midsole prevents excessive bending, especially helpful in managing pain for Plantar Fasciitis.
Choosing Shoes Based on Activity
Different lifestyles and daily routines require different shoe features. Here’s a breakdown based on typical activity types:
🌿 Everyday Walking
Orthotic-compatible slip-ons or supportive sneakers
Cushion-focused footbeds with arch elevation
Deep heel cups for alignment
🏋️ Exercise and Sports
Athletic shoes with reinforced heel counters
Lateral support for high-arched feet
Even if you haven’t been formally diagnosed, your shoes might be causing—or worsening—foot conditions. Watch out for:
Outsoles worn more on one side
Pain that fades when barefoot
Tingling or numbness in toes
Shoes that “tilt” when placed on a flat surface
Pain that gets worse throughout the day
Custom Orthotics: Do You Need Them?
If over-the-counter footwear isn’t enough, a podiatrist might recommend custom orthotics—personalized inserts that offer enhanced support. These are especially helpful if you:
Have severe foot deformities
Experience recurring ankle instability
Have one leg longer than the other (common with Per Cavus)
However, orthotic shoes aren’t always necessary if you select well-designed, ergonomic footwear in the first place.
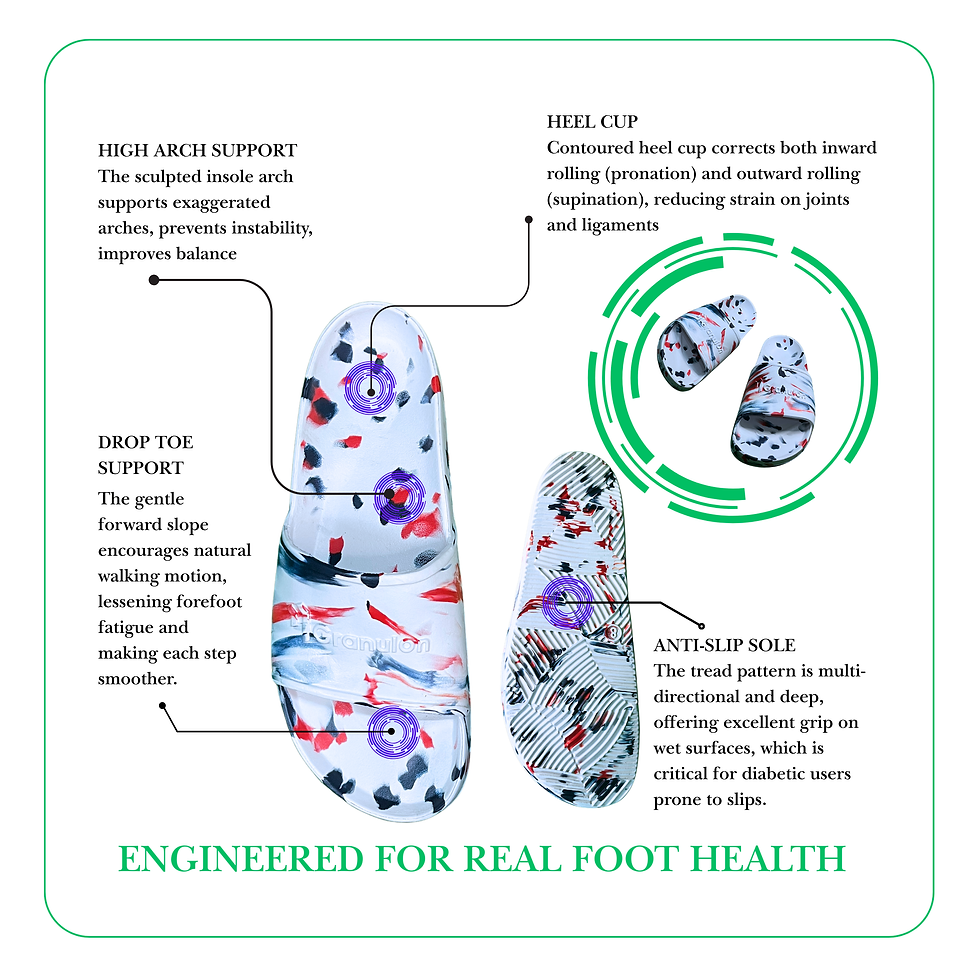
Granulon G1: One Small Mention, One Big Difference
For those seeking footwear that blends support, comfort, and style—Granulon G1 offers high-arch support in a lightweight slide, engineered with a Phylon midsole for long-day relief. While we don’t push it as a medical device, customers with foot pain have found it exceptionally comfortable.
(Just 45 words, as you asked.)
Beyond Shoes: Lifestyle Changes That Help
Correct footwear is just one part of the puzzle. Managing these foot conditions often requires a more holistic approach.
Stretching & Strengthening
Calf stretches
Plantar fascia roll with a frozen bottle
Towel toe curls
Ankle mobility drills
Weight Management
Losing excess weight can reduce pressure on the plantar fascia and forefoot.
Physical Therapy
Especially helpful for Per Cavus where gait retraining and balance exercises improve mobility.
Night Splints & Compression Socks
Aid in maintaining foot posture during rest and support circulation.
When to See a Specialist
Foot pain shouldn't be ignored—especially if it interferes with daily function. Consult a podiatrist if:
Pain persists for more than two weeks
Over-the-counter insoles or shoes provide no relief
You notice foot deformities or changes in skin color
You experience numbness, weakness, or tingling
Early intervention can prevent long-term damage and help avoid more invasive treatments like injections or surgery.
Final Thoughts: Step into Support
Living with Plantar Fasciitis or Per Cavus doesn’t mean giving up on comfort or mobility—it just means making smarter, more informed decisions. Footwear is the most impactful and accessible way to manage these conditions on a daily basis.
When you choose the right shoes, you don’t just support your feet—you support your entire body, lifestyle, and long-term health. Whether it's an everyday slide like Granulon G1 or a tailored orthotic insert, investing in foot health is investing in your future mobility.
Because every step counts—and it's time yours felt better.


Comments